Nigeria’s healthcare system is facing a severe manpower crisis, with the number of practising doctors now standing at approximately 40,000—far short of the estimated 300,000 needed to serve a population of over 220 million.
Recent disclosures by health authorities highlight a sharp decline in the medical workforce, largely driven by the sustained emigration of healthcare professionals, commonly known as the japa phenomenon.
In 2024, the Minister of Health and Social Welfare, Prof. Muhammad Pate, revealed that Nigeria had approximately 55,000 licensed doctors.
He also disclosed that at least 16,000 doctors had left the country within five years, while about 17,000 others had moved out of active clinical service.
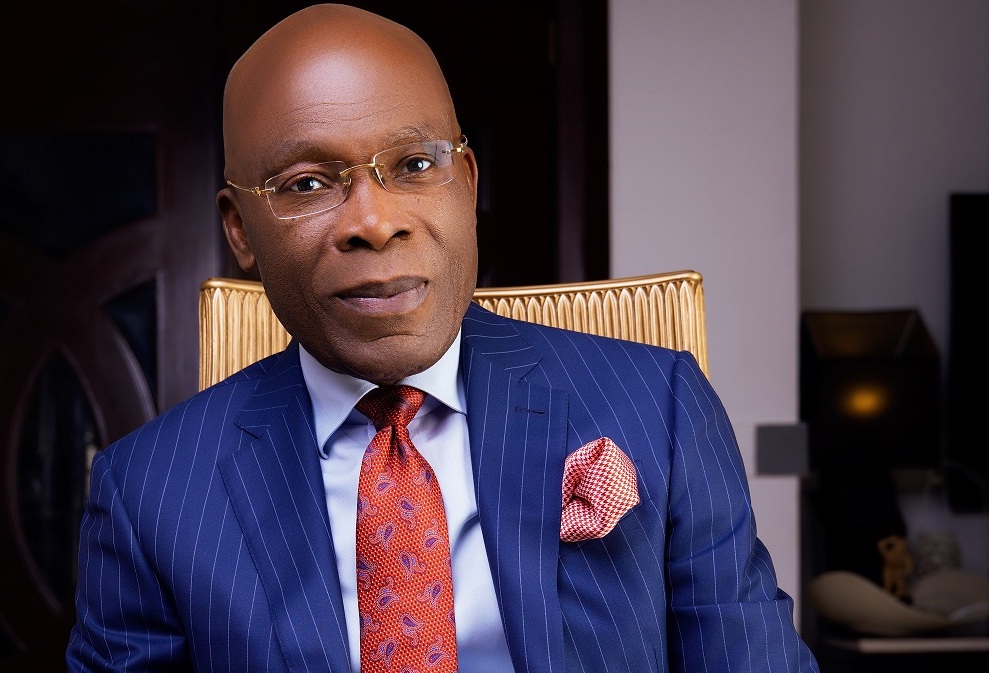
However, new data from the Lagos State Commissioner for Health, Prof. Akin Abayomi, shows that the number has further declined to about 40,000 practising doctors nationwide within just one year.
Abayomi made this disclosure during a presentation at a leadership dialogue in Lagos themed “Strengthening Primary Healthcare Systems: A Joint Leadership Dialogue.”
“Nigeria currently has about 40,000 doctors, yet the country requires no fewer than 300,000 to meet the healthcare needs of its population,” Abayomi said.
He noted that Lagos State, the country’s most populous state, is among the hardest hit by the shortage.
“Lagos has only about 7,000 doctors serving an estimated population of nearly 30 million people. To function optimally, the state requires at least 33,000 doctors,” he added.
According to him, the widening doctor-to-population gap has placed enormous pressure on the existing workforce and weakened healthcare delivery, particularly at the primary healthcare level.
To address the challenge, Abayomi said the Lagos State Government is investing heavily in its newly established University of Medicine and Health.
“Within the next five years, the university is expected to produce about 2,500 healthcare professionals annually, including doctors, laboratory scientists, and other critical health workers,” he said.
The persistent migration of medical professionals continues to raise serious concerns within the health sector.
A 2017 survey conducted by a Nigerian polling organisation in collaboration with Nigeria Health Watch found that nearly 88 per cent of Nigerian doctors were actively seeking employment opportunities abroad.
Healthcare experts have attributed the worsening brain drain to poor funding, inadequate infrastructure, insecurity, harsh working conditions, and weak implementation of existing health policies.
Data from the United Kingdom’s General Medical Council shows that 11,001 Nigerian-trained doctors are currently practising in the UK, highlighting the scale of the exodus.
The President of the Nigerian Medical Association, Prof. Bala Audu, recently warned that Nigeria has moved beyond passive brain drain and has become a direct recruitment ground for foreign governments.
“International recruiters now come into Nigeria to recruit doctors directly, especially specialists such as obstetricians, gynaecologists, and paediatricians,” Audu said.
“They offer better pay, modern infrastructure, and improved working conditions, which our system currently struggles to provide.”
Audu expressed concern that the loss of skilled professionals is happening at a time when Nigeria’s population and healthcare demands are rising.
“We are recording more births, yet maternal mortality remains high because the specialists needed to manage these cases are leaving in large numbers,” he added.
He further revealed that in some medical specialties, more Nigerian doctors may now be practising abroad than within the country.
Similarly, a former President of the NMA, Prof. Mike Ogirima, described Nigeria’s doctor-to-patient ratio as “alarming,” noting that the country currently has about one doctor to 8,000 patients—far below the World Health Organisation’s recommendation of one doctor to 600 patients.
“Nigeria produces an average of about 3,000 doctors annually. At that rate, it would take many years to bridge the gap, even if no doctor leaves the system,” Ogirima said.
“That reality explains why doctors are overstretched, burned out, and increasingly frustrated.”
Ogirima urged the government to prioritise investment in medical training, improve security, and equip health facilities with modern tools, warning that retention would remain difficult without meaningful reforms.
Medical professionals have continued to call on federal and state governments to urgently address welfare concerns, including comprehensive insurance coverage and improved working conditions, stressing that a motivated and protected health workforce is critical to national development.